Renew Life at the Cellular Level Advanced Bone Marrow Transplant Care for Blood Disorders and Cancer
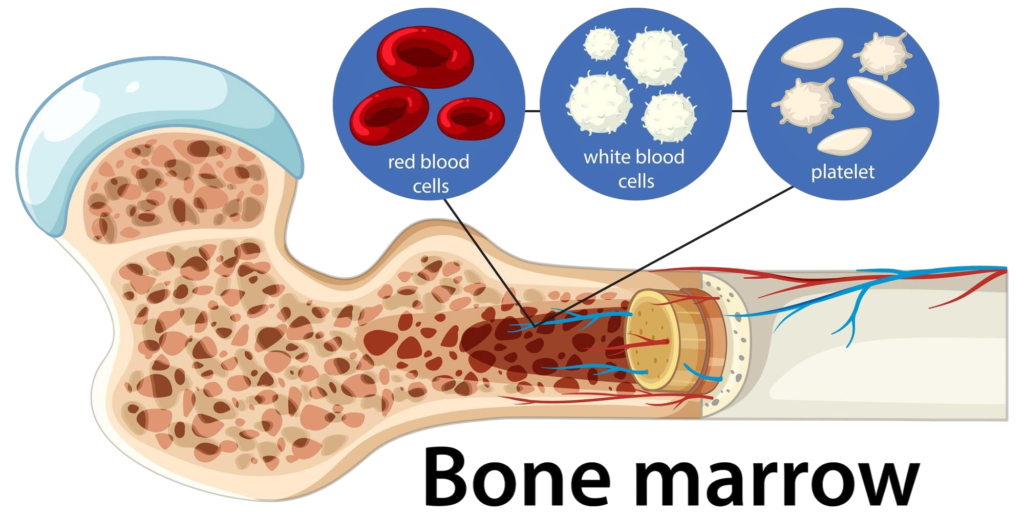
A bone marrow transplant (BMT), also known as a hematopoietic stem cell transplant (HSCT), is a medical procedure used to replace diseased or damaged bone marrow with healthy stem cells. Bone marrow is the soft, spongy tissue inside bones responsible for producing blood cells, including red blood cells, white blood cells, and platelets. When bone marrow is damaged or defective, the body cannot produce healthy blood cells, leading to life-threatening conditions.
Bone marrow transplantation is commonly indicated for:
- Blood cancers such as leukemia, lymphoma, and multiple myeloma
- Genetic blood disorders like sickle cell anemia and thalassemia
- Bone marrow failure syndromes such as aplastic anemia
- Immune deficiencies that prevent proper production of white blood cells
By replacing defective marrow with healthy stem cells, BMT can restore normal blood cell production, rebuild the immune system, and, in many cases, cure life-threatening diseases.
Types of Bone Marrow Transplant
There are two main types of BMT:
- Autologous Transplant:
The patient’s own stem cells are harvested, treated, and reinfused after high-dose chemotherapy. This method is typically used for certain types of lymphoma and multiple myeloma.
- Allogeneic Transplant:
Stem cells are obtained from a compatible donor (related or unrelated). This type is necessary for conditions where the patient’s marrow is genetically defective or destroyed by disease.
Stem cells can be obtained from:
- Bone marrow (traditional method)
- Peripheral blood (after stimulating stem cells to move into blood)
- Umbilical cord blood (used in pediatric or rare cases)
Book An Appointment
Evaluation and Preparation
Before undergoing a BMT, patients undergo a thorough evaluation to determine eligibility, minimize risks, and prepare for intensive treatment. The evaluation process includes:
- Disease assessment – diagnosis, staging, and previous treatments
- Organ function tests – heart, liver, kidney, and lung function
- Infectious disease screening – to detect latent infections that could complicate transplant
- Immunologic testing – for allogeneic transplants, to ensure donor compatibility
- Psychosocial assessment – evaluating patient readiness, support systems, and ability to adhere to post-transplant care
Patients then receive conditioning therapy, typically high-dose chemotherapy or radiation, to destroy diseased marrow, suppress the immune system, and make room for the new stem cells.
The Bone Marrow Transplant Procedure
The transplant procedure itself is relatively straightforward: stem cells are infused into the patient’s bloodstream through a central line, similar to a blood transfusion. These stem cells then migrate to the bone marrow and begin producing healthy blood cells, a process called engraftment.
- Hospitalization: Typically lasts 3–6 weeks depending on complications
- Isolation precautions: Patients are often kept in protective isolation to prevent infections due to severely compromised immunity
- Supportive care: Includes transfusions, antibiotics, antivirals, nutrition support, and management of side effects
Engraftment usually occurs within 2–4 weeks, but full immune recovery may take months. During this time, patients require intensive monitoring for infections, graft-versus-host disease (GVHD), or complications from conditioning therapy.
Post-Transplant Care and Long-Term Monitoring
After discharge, lifelong follow-up is essential to monitor:
- Blood cell counts and immune function
- Signs of graft-versus-host disease (for allogeneic transplants)
- Late effects such as organ dysfunction, secondary cancers, or endocrine issues
Post-transplant recovery involves:
- Gradual resumption of normal activities
- Nutrition counseling to strengthen immunity
- Vaccinations to rebuild immunity
- Adherence to medications, including immunosuppressants (for allogeneic transplants)
With careful monitoring and supportive care, BMT offers patients the potential for complete remission of their disease and restoration of normal blood and immune function.
Meet Our Experts
Our hematologists and transplant specialists are experienced in managing complex blood disorders and transplant cases, supported by dedicated nursing and critical care teams focused on patient safety and recovery.

CH CHAKRADHAR REDDY
SR. Orthopeadic Surgeon
MBBS, MS (ORTHOPAEDICS), FIAP (INDIA), FIAS (ITALY)

SUJITKUMAR VAKATI R
SR. Orthopeadic Surgeon
Ms.Ortho , Mch.Ortho A.A.F , S.E.F, AOT, IWC, Dip. In Football Medicine (FIFA)


Outcomes and Quality of Life
Bone marrow transplantation can be curative for many blood disorders, with survival and success rates improving steadily due to advances in:
- Donor matching techniques
- Conditioning regimens
- Infection prevention and supportive care
- GVHD management
Patients often experience:
- Restoration of normal blood counts
- Improved energy and immunity
- Freedom from frequent hospital treatments
- Enhanced quality of life and independence
Long-term success depends on adherence to follow-up care, monitoring for late complications, and a strong support system.
FAQ's
Who is eligible for a bone marrow transplant?
Patients with blood cancers, bone marrow failure syndromes, or genetic blood disorders.
What is the difference between autologous and allogeneic transplant?
Autologous uses the patient’s own stem cells; allogeneic uses a donor’s stem cells.
How long does recovery take?
Hospital stay is 3–6 weeks; immune recovery may take 6–12 months.
What complications can occur?
Infection, bleeding, graft-versus-host disease, organ toxicity, and relapse of the original
Disease.
Will I need medications after transplant?
Yes immunosuppressive therapy is required for allogeneic transplants, along with supportive medications.