When the Heart Fails, Life Begins Anew Advanced Heart Transplant Care with Compassion and Expertise
A heart transplant is one of the most complex and life-saving surgical procedures in modern medicine. It involves replacing a diseased or failing heart with a healthy donor heart, offering a new lease on life for patients with end-stage heart failure or severe cardiac conditions that no longer respond to medication, devices, or other therapies. Heart transplantation is often considered when a patient’s quality of life is severely compromised, and the risk of mortality without intervention is high.
Why Heart Transplant Is Needed
Heart failure is a progressive condition in which the heart cannot pump blood effectively, leading to symptoms like shortness of breath, fatigue, swelling in legs, and persistent fluid retention. In advanced stages, patients may experience life-threatening arrhythmias, cardiogenic shock, or multi-organ dysfunction, which cannot be managed with medications, pacemakers, or ventricular assist devices alone. In such cases, a heart transplant becomes the only viable option to restore functional cardiac output and improve survival.
Common conditions requiring heart transplant include:
- Dilated cardiomyopathy – weakened heart muscle causing reduced pumping efficiency.
- Ischemic heart disease – extensive damage from heart attacks that leaves the heart unable to meet the body’s demands.
- Congenital heart defects – certain structural abnormalities may lead to end-stage heart failure.
- Refractory heart failure – patients who fail to respond to optimal medical therapy, devices, or surgery.
Evaluation and Preparation for Heart Transplant
Becoming eligible for a heart transplant involves a comprehensive evaluation by a multidisciplinary team, including cardiologists, transplant surgeons, infectious disease specialists, nephrologists, nutritionists, and psychologists. The assessment ensures that the patient is medically fit for surgery and post-operative recovery, and that potential risks are minimized.
Key components of evaluation include:
- Cardiac function tests – echocardiography, MRI, and stress testing assess heart performance.
- Hemodynamic evaluation – right heart catheterization measures pressures and evaluates pulmonary function.
- Organ function screening – liver, kidney, and lung function tests ensure other organs can tolerate surgery.
- Infection and immunology screening – identifies latent infections and assesses compatibility for immunosuppressive therapy.
- Psychosocial assessment – evaluates patient readiness, support systems, and adherence potential for post-transplant care.
Once deemed suitable, patients are placed on a donor waiting list, where allocation is based on urgency, blood type, body size, and tissue compatibility. Advances in organ preservation and allocation systems ensure the highest chance of matching suitable donor hearts with waiting patients.
Book An Appointment
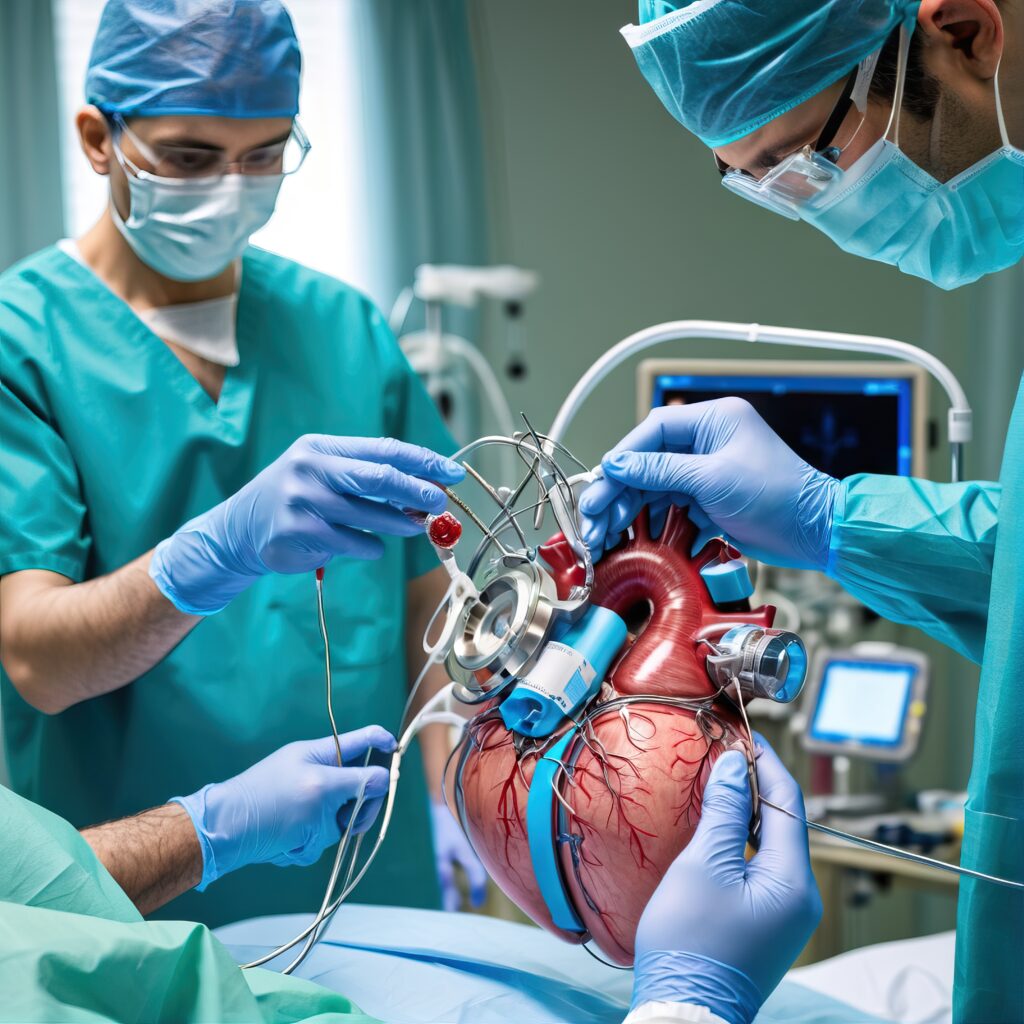
The Heart Transplant Procedure
Heart transplantation is performed under general anesthesia and usually lasts 4–6 hours. The surgeon removes the failing heart and implants the donor heart, carefully reconnecting all major blood vessels, including the aorta, pulmonary arteries, and veins. After surgery, patients are closely monitored in the Intensive Care Unit (ICU) to ensure the new heart functions effectively and to manage immediate post-operative risks.
Modern techniques focus on minimizing ischemia time, optimizing surgical precision, and improving patient outcomes. Advances in immunosuppressive therapy reduce the risk of organ rejection, while early mobilization and rehabilitation programs enhance recovery. Patients are educated on heart-healthy lifestyles, medication adherence, and monitoring for signs of rejection.
Post-Transplant Care and Long-Term Outlook
After a heart transplant, patients are typically hospitalized for 1–2 weeks, followed by a structured outpatient program including:
- Immunosuppressive therapy – lifelong medications to prevent rejection.
- Regular monitoring – blood tests, echocardiograms, and biopsies to detect early signs of rejection.
- Rehabilitation – cardiac rehab, nutrition counseling, and exercise programs to improve cardiovascular health.
- Psychological support – managing the emotional and mental health aspects of transplantation.
Survival rates have improved significantly in the last two decades. Many patients live 10–15 years or longer post-transplant, with improved quality of life, energy levels, and functional capacity. Success depends on patient adherence to medications, lifestyle management, and regular follow-up care.
Heart transplantation is not only a surgical procedure it is a lifesaving journey requiring the collaboration of patients, families, and a dedicated transplant care team. At centers of excellence, such as Urban Hospitals, every aspect of the journey is personalized to maximize outcomes and provide compassionate, human-centered care.
Meet Our Experts
Our hematologists and transplant specialists are experienced in managing complex blood disorders and transplant cases, supported by dedicated nursing and critical care teams focused on patient safety and recovery.

CH CHAKRADHAR REDDY
SR. Orthopeadic Surgeon
MBBS, MS (ORTHOPAEDICS), FIAP (INDIA), FIAS (ITALY)

SUJITKUMAR VAKATI R
SR. Orthopeadic Surgeon
Ms.Ortho , Mch.Ortho A.A.F , S.E.F, AOT, IWC, Dip. In Football Medicine (FIFA)


FAQ's
Who is eligible for a heart transplant?
Patients with end-stage heart failure unresponsive to medication or devices, or those with life-threatening cardiomyopathy.
How long is recovery after surgery?
Initial hospitalization is 1–2 weeks; full recovery can take 3–6 months with rehabilitation.
Is lifelong medication required?
Yes immunosuppressive therapy is essential to prevent organ rejection.
What lifestyle changes are recommended?
Heart-healthy diet, regular exercise, infection prevention, stress management, and regular follow-ups.
What are the risks associated with heart transplant?
Risks include organ rejection, infection, complications from surgery, and medication side effects.